publication / February 12, 2026
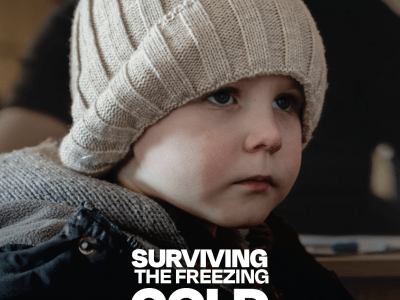
Surviving the Freezing Cold Under Fire: How Winter Disrupts Education and Mental Health Support for Ukrainian Children
As winter hardship intensifies in Ukraine, 100% of surveyed families report extreme conditions where a lack of heat, electricity, and education is pushing children to a breaking point. This briefing outlines the urgent need for flexible funding and support to protect families from a cumulative humanitarian crisis.
article / February 23, 2026
World Vision Ghana Leads Regional Town Hall on NTD Elimination in Oti Region
World Vision Ghana, the Ministry of Health and GHS convene a Regional Town Hall Meeting in the Oti Region to strengthen sub-national ownership in the elimination of Neglected Tropical Diseases.
article / February 25, 2026
Community health workers in Ouallam: silent guardians strengthening epidemic response
In Ouallam, 39 community health workers support families daily despite insecurity and scarce resources. According to Souleymane Idrissa, head of the Ouallam health center, trainings provided through the “Strengthening access to care and epidemic control” project funded by World Health Organization and implemented by World Vision Niger and ISCV marked a major turning point. Health workers gained critical skills in managing gender-based violence, encouraging referrals, and supporting survivors, including access to psychological care.
The project also strengthened disease surveillance through training on the minimum emergency activity package, enabling faster detection and reporting of measles, malaria, cholera, meningitis, and other serious illnesses, even in displaced persons sites. Long-serving relays like Seyni Seydou and Maimouna Birgui describe a deepened sense of purpose, improved knowledge, and stronger community trust.
Beyond technical skills, the trainings enhanced awareness-raising, early care-seeking, and social cohesion. Today, community health workers in Ouallam act as true health sentinels, better equipped to prevent disease, respond to epidemics, and protect their communities.
article / February 23, 2026
A Mother, 25 Taka, and a Promise to Protect Her Children’s Health in Ramu
In Ramu, Cox’s Bazar, a mother improves her children’s health through safe water, hygiene awareness, and access to a sanitary toilet.
article / February 9, 2026
A journey of Change: How Social Accountability transformed Svay Ta Yean Health Centre
Svay Ta Yean Health Center, once plagued by poor infrastructure, low patient turnout, and weak accountability, has undergone a remarkable transformation through the Implementation of the Social Accountability Framework (I-SAF). In early 2023, under the leadership of Mr. Chan Boran and with support from STAR Kampuchea, community feedback was gathered through scorecards, interface meetings, and joint action plans, sparking major improvements in service delivery, transparency, and infrastructure. Today, the health center operates 24/7, treats patients with dignity, and actively engages with the community. Monthly patient visits have tripled, and deliveries have increased significantly. Residents praise the staff’s professionalism and kindness, while management commits to sustaining progress through continuous collaboration and accountability. What was once a struggling facility is now a trusted hub of quality healthcare and citizen engagement.
article / February 25, 2026
Reaching the unreachable: how mobile clinics transformed access to care in Gaya
Before the project, access to healthcare in the Gaya area was extremely limited. Many isolated villages forced vulnerable families to walk for hours to reach health centers in Tounouga or Gaya, often arriving too late for proper treatment. The situation was worsened by seasonal floods in Dosso and Tillaberi, which cut off communities and left thousands without essential health services. According to Mrs. Edui Ramatou, Head of the Gaya 2 Health Center, common illnesses such as malaria, diarrhea, and respiratory infections were difficult to manage due to limited supplies and reliance on only two small health posts.
In response, World Health Organization supported the project “Anticipatory health assistance for at-risk and flood-affected populations,” implemented by World Vision Niger and ISCV. Completed in May 2025, the project introduced mobile clinics that brought care directly to villages. Monthly consultations increased from 1,000 to 1,800, while trained community health workers improved case detection and follow-up. For mothers, children, the elderly, and pregnant women, access to timely care greatly improved. Although the project ended, its positive impact continues, and communities hope for sustained support to strengthen resilience against future floods.
article / February 19, 2026
World Vision’s Integrated Programs Transform Learning, Health, and Hope for 1,052 Learners in Pitseng
World Vision’s integrated programs transformed a primary school in Pitseng, providing clean water, safe toilets, new classrooms, school gardens, and poultry projects, improving learning, hygiene, and student wellbeing