article / February 25, 2026
Protecting Tomorrow: A Family’s Fight Against Malaria
In Zambezia Province, rising malaria cases threaten families like Samuel and Carolina’s, with over 311,000 cases recorded in Mocuba District in 2025 alone. Through a Global Fund–supported insecticide-treated nets campaign, led by World Vision and partners, millions of mosquito nets are being distributed across Mozambique, protecting children, supporting pregnant women, and giving families renewed hope for a healthier future.
article / February 25, 2026
Community health workers in Ouallam: silent guardians strengthening epidemic response
In Ouallam, 39 community health workers support families daily despite insecurity and scarce resources. According to Souleymane Idrissa, head of the Ouallam health center, trainings provided through the “Strengthening access to care and epidemic control” project funded by World Health Organization and implemented by World Vision Niger and ISCV marked a major turning point. Health workers gained critical skills in managing gender-based violence, encouraging referrals, and supporting survivors, including access to psychological care.
The project also strengthened disease surveillance through training on the minimum emergency activity package, enabling faster detection and reporting of measles, malaria, cholera, meningitis, and other serious illnesses, even in displaced persons sites. Long-serving relays like Seyni Seydou and Maimouna Birgui describe a deepened sense of purpose, improved knowledge, and stronger community trust.
Beyond technical skills, the trainings enhanced awareness-raising, early care-seeking, and social cohesion. Today, community health workers in Ouallam act as true health sentinels, better equipped to prevent disease, respond to epidemics, and protect their communities.
article / January 15, 2026
Protecting Young Lives: Mozambique’s Renewed Fight Against Malaria
Children under five bear the greatest burden of malaria in Tete. Explore renewed commitments, innovations, and community action to end malaria.
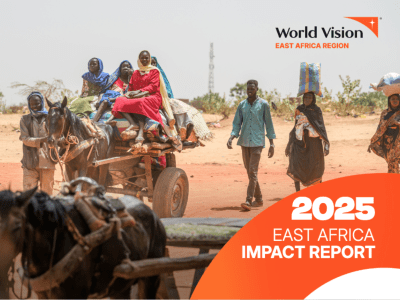
publication / February 23, 2026
World Vision East Africa Impact Report 2025
Despite escalating conflict, climate shocks, economic instability and widespread displacement, we reached over 26 million people, including 16.4 million children
article / February 11, 2026
DR Congo: Fungurume Under Water: A Dual-Risk Crisis Requiring a Rapid, Child-Centred Response
This article highlights the severe flooding that struck Fungurume in Lualaba Province, Democratic Republic of the Congo, on 1 February 2026, affecting more than 3,200 people. Occurring in the midst of an ongoing cholera outbreak, the disaster has created a dual emergency, increasing risks of waterborne diseases, malaria, school disruption, and child protection concerns. With homes, schools, and health centres inundated, families face heightened vulnerability, particularly children. The article underscores the need for a rapid, coordinated, and child-centred humanitarian response focused on health, WASH, education continuity, shelter, and protection to prevent a worsening secondary crisis.
article / February 9, 2026
Finding Courage in Care: Leah’s Journey to Women’s Health
World Vision’s outreach clinics bring women’s health education and VIA screening closer to communities, transforming lives like Leah’s in Solomon Islands.
article / February 23, 2026
A Mother, 25 Taka, and a Promise to Protect Her Children’s Health in Ramu
In Ramu, Cox’s Bazar, a mother improves her children’s health through safe water, hygiene awareness, and access to a sanitary toilet.