article / February 19, 2026
Strengthening Emergency Delivery Care in the West Bank: 121 Health Workers Trained Against All Odds
In August 2025, World Vision, in close partnership with the Ministry of Health (MoH), delivered a three‑week Emergency Delivery Training programme, equipping 121 nurses, doctors, and midwives with the skills needed to respond to maternal and newborn emergencies.
article / February 19, 2026
World Vision’s Integrated Programs Transform Learning, Health, and Hope for 1,052 Learners in Pitseng
World Vision’s integrated programs transformed a primary school in Pitseng, providing clean water, safe toilets, new classrooms, school gardens, and poultry projects, improving learning, hygiene, and student wellbeing
publication / February 12, 2026
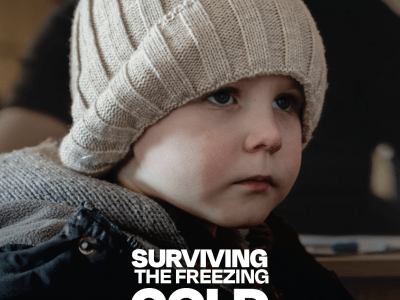
Surviving the Freezing Cold Under Fire: How Winter Disrupts Education and Mental Health Support for Ukrainian Children
As winter hardship intensifies in Ukraine, 100% of surveyed families report extreme conditions where a lack of heat, electricity, and education is pushing children to a breaking point. This briefing outlines the urgent need for flexible funding and support to protect families from a cumulative humanitarian crisis.
opinion / February 20, 2026
Mozambique’s Children Are Paying the Price for a Crisis They Didn’t Create
Juma Ignatius, Senior Policy Advisor, Climate Action and Disaster Risk Reduction, Disaster Management, brings our attention to the recent Mozambique floods that are often framed as natural disasters, but in reality, it is a story of global inequality, climate inaction and decades of neglect paid for by children who did nothing to cause the crisis. As emergency aid is repeated and preparedness is ignored, based on the negotiations within the UNFCCC spaces, Juma argues that without a shift to Disaster Risk Reduction, Anticipatory Action and climate-resilient development, disasters will continue to steal childhoods.
article / February 5, 2026
Clean Water Improves Maternal Care at Nambazo Health Centre in Phalombe
Clean and safe water is transforming maternal health at Nambazo Health Centre in Phalombe, as World Vision Malawi’s WASH project reduces infections and improves dignity.
article / February 9, 2026
A journey of Change: How Social Accountability transformed Svay Ta Yean Health Centre
Svay Ta Yean Health Center, once plagued by poor infrastructure, low patient turnout, and weak accountability, has undergone a remarkable transformation through the Implementation of the Social Accountability Framework (I-SAF). In early 2023, under the leadership of Mr. Chan Boran and with support from STAR Kampuchea, community feedback was gathered through scorecards, interface meetings, and joint action plans, sparking major improvements in service delivery, transparency, and infrastructure. Today, the health center operates 24/7, treats patients with dignity, and actively engages with the community. Monthly patient visits have tripled, and deliveries have increased significantly. Residents praise the staff’s professionalism and kindness, while management commits to sustaining progress through continuous collaboration and accountability. What was once a struggling facility is now a trusted hub of quality healthcare and citizen engagement.
publication / February 17, 2026
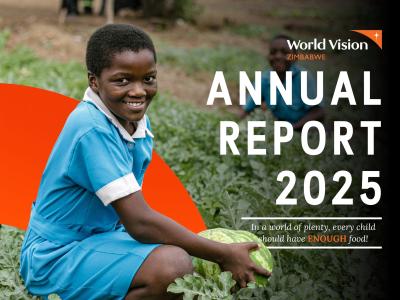
World Vision Zimbabwe 2025 Annual Report
In this 2025 Annual Report, discover powerful stories that highlight World Vision Zimbabwe's (WVZ) transformative impact on the lives of the most vulnerable children. Driven by an unshakable dedication to championing the well-being of girls and boys in need, we are strategically refocusing and amplifying our efforts to tackle extreme vulnerability head-on.