Our top ten calls for improved mental health care for the Middle East and Eastern Europe
“Mental health is a universal human right” might be the theme for this year’s #WorldMentalHealthDay, but Mike Kirakossian reminds us, it’s not a right shared by everyone.
The Middle East and Eastern Europe region includes a wide range of cultural, socioeconomic, and political contexts, each with its own implications for mental health. According to the World Health Organization, the region has a high rate of mental conditions, with an estimated 17.6% of the population living with at least one mental or substance use condition. This is hardly surprising when much of the region faces armed conflicts, displacement, poverty, inequality, and human rights violations that all exacerbate mental health problems.
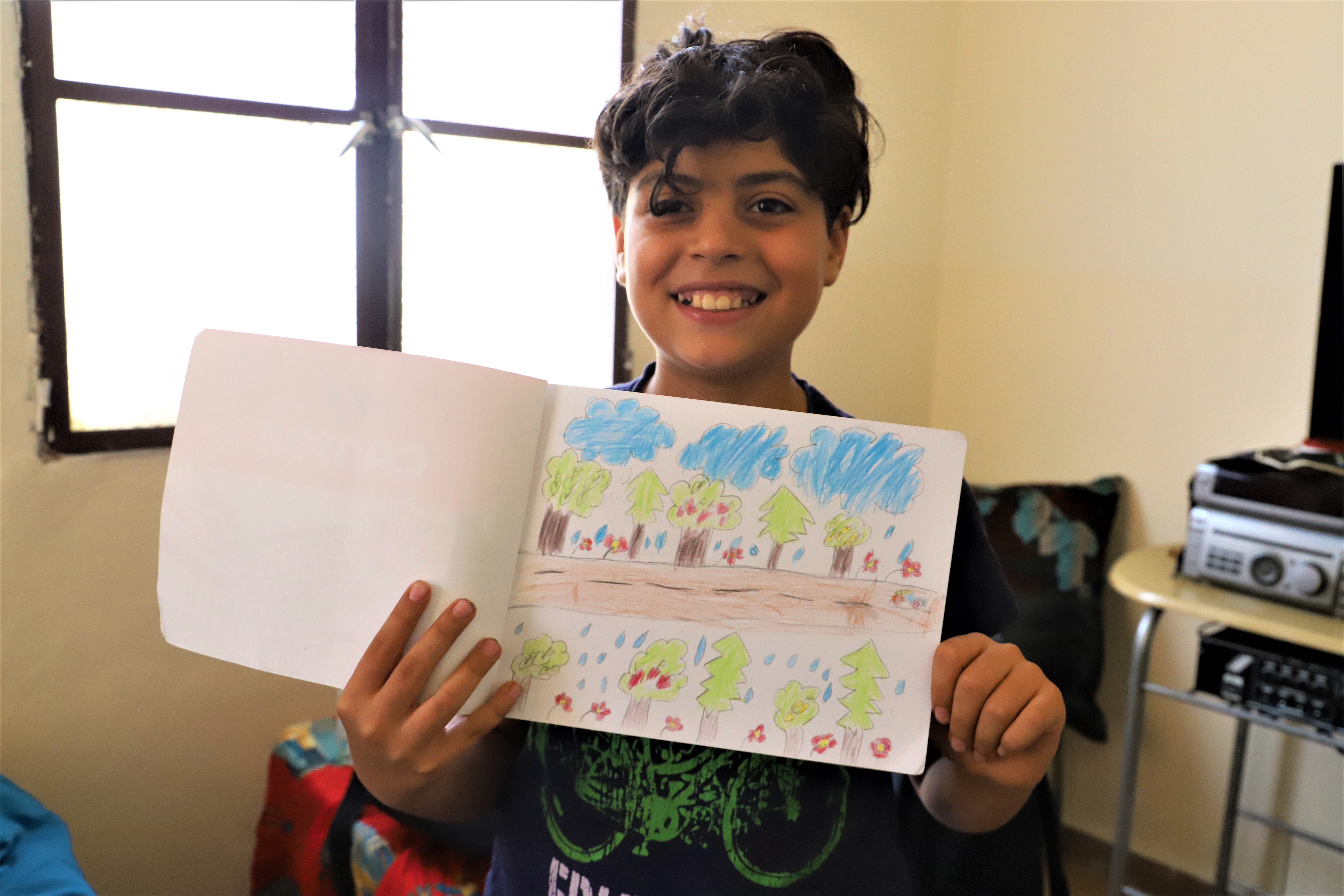
Children's needs are particularly important to consider, as they are disproportionately affected by conflict, displacement, and other forms of adversity. Children are especially vulnerable to the mental health consequences of conflict, displacement, and other forms of adversity. As our report on the children of Ukraine revealed, children may experience trauma, grief, and loss, as well as disruptions to their education, social support networks, and routines. These experiences can have a profound impact on their mental and emotional well-being, both in the short-term and long-term.

Acknowledging the differences
Ensuring mental health equity in this region requires a nuanced and contextualised approach, taking into account the varying needs, as well as addressing the multiple and intersecting forms of discrimination and marginalisation, such as gender, ethnicity, sexual orientation, religion, and disability.
Major mental health accessibility across the region faces the following obstacles:
- Lack of adequate infrastructure and resources
- Artificial separation between mental and physical health
- Geographical distance and isolation, especially those who are displaced and/or living in rural, remote or conflict areas
- Stigma and discrimination
- Lack of supportive and enabling environment that promotes and protects mental wellbeing
- Lack of political will and commitment to prioritise mental health as a universal right
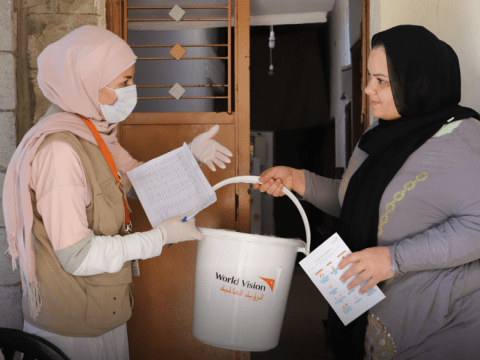
To counter these challenges, World Vision is investing in people, infrastructure, equipment, and technology to provide access to child-friendly mental health and psychosocial assessment and support. Across the region we are advocating for inclusive, accessible and affordable mental health policies and programmes, working with communities to raise awareness and reduce stigma and developing and implementing mental health and psychosocial care programs for children, youth, and adults.
Boosting our efforts
World Vision is renewing our commitment to integrate mental health psychosocial support (MHPSS) into all sectors and budgets across the Middle East and Eastern Europe. We will continue to build staff and partner MHPSS capacity, provide MHPSS support for displaced populations and strengthen existing community-based services, or establish new ones. We will deploy MHPSS services to cater to individuals with specific needs, build resilience and nurture coping mechanisms through psychosocial support. Our staff and partners will provide life skills training and parenting support programmes, we will invest in long-term planning and research, and strengthen collaboration and partnerships with local stakeholders. To ensure efficient and impactful programming we will continuously monitor and learn from our ongoing efforts to adapt and improve interventions.
Calling for changes
But more needs to be done. World Vision staff are also championing the following interventions from the sector and international community:
- Increasing the availability, accessibility, affordability, and quality of mental health services. This includes investing in mental health professionals skilled in working with children and their diverse mental health and psychosocial needs.
- Incorporation of mental health into primary health care, which is the first point of contact for most people seeking health services in order to detect and address mental health issues early before they become more severe or chronic and reduces barriers of cost, distance, and stigma.
- Leveraging technology to extend reach and impact of mental health services and enable access to mental health care from a distance, without having to travel or face security risks.
- Greater provision of telehealth resources facilitates to increase collaboration and consultation among mental health professionals, as well as the supervision and training of primary health care workers.
- Improve the ability for people to access digital platforms that provide information, self-help tools, peer support,and advocate for mental health rights.
- Enhance the training, supervision, and retention of mental health professionals through offering specialized training programs in child mental health, providing opportunities for mental health professionals to supervise and mentor each other, and creating supportive work environments for mental health professionals who work with children.
- Adequate and sustainable funding for mental health programs and policies through funding mental health services in schools and other community settings, supporting programs that promote mental health and well-being in children, and investing in research on the mental health and psychosocial needs of children and the effectiveness of different interventions.
- Conduct public awareness campaigns that increase knowledge, understanding, and empathy towards mental health issues and empowering people with lived mental health experience, their families and carers.
- The development and implementation of laws, policies, and strategies that champion mental health parity, protect against discrimination and human rights violations, and allocate resources and accountability mechanisms for mental health services and programs.
- Advocacy initiatives, from individual to collective, from local to global, from informal to formal, that raise awareness, mobilizes support, influences policies, or monitors progress.
As World Vision marks World Mental Health Day 2023 in the Middle East and Eastern Europe region, we are reminded that through our global strategy we have made promises to the children we serve that they should live life in all its fullness. An important part of this promise is promoting better mental health. By removing barriers and fostering equity, we can pave the way for a future where mental health and psychosocial well-being is not a privilege but a universal right.
To learn more about World Vision’s work in the Middle East and Eastern Europe click here
Mike Kirakossian is World Vision, MHPSS Adviser in the Middle East and Eastern Europe regional office, based in Beirut, Lebanon. He joined World Vision in 2019. Mike holds a bachelor's degree in psychology and a master's degree in clinical and adjustment psychology. He is a licensed practitioner specialising in trauma-informed care, psychosocial interventions for children, youth and adults, emotional crisis management, harmful use of substance prevention, and response programs utilizing the Integrative Approach in his clinical work. He has 9 years of experience in humanitarian, development, and peacebuilding work with reputable national and international organizations, where he focuses on Mental Health and Psychosocial Support, Child Protection, Gender-Based Violence, Disability Inclusion programming, research, and integration. Mike also serves as the regional psychosocial consultant supporting IFRC staff and delegates in the Middle East and North Africa region.