Resilience in the Rubble: Mental Health as the Foundation of Sustainable Recovery
Phiona Koyiet, Senior Technical Advisor for Mental Health and Psychosocial, calls for more investment in mental health and psychological well-being in emergencies, ensuring children and communities in the most fragile and crisis-affected settings can not only survive, but thrive.
10 October 2025
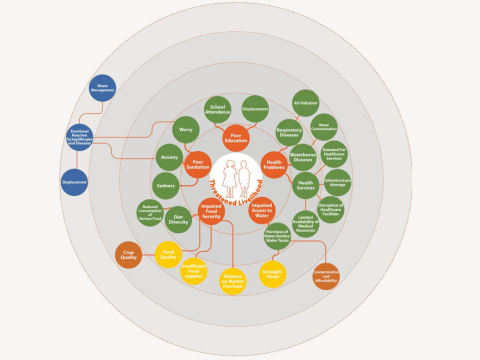
Against the backdrop of humanitarian emergencies, mental health becomes not a luxury but a critical lifeline. Crises — whether conflict, natural disaster, or public health emergency — not only threaten lives and infrastructure, but they also tear at the very fabric of communities and minds.
This is especially true for vulnerable children and communities who face multiple stressors, loss, displacement, and emotional and social problems. Investing in mental health services in these settings is not just a moral imperative, it is foundational to achieving the Sustainable Development Goals (SDGs). Because without psychological resilience, recovery, stability, and development are at risk.

The statistics are staggering
For children, who are among the most vulnerable population in a crisis or disaster, poor mental health not only hinders their learning and development but is a top cause of death, disease and disability, especially for older adolescents.
1 in 5 people in post-conflict settings has depression, anxiety disorders, post-traumatic stress disorders, bipolar disorders, or schizophrenia. 1 in 10 people has a moderate or severe mental disorder at any point in time.
According to WHO, refugees and migrants exposed to adversity are more likely than host populations to experience mental health conditions such as depression, anxiety, post-traumatic stress disorder, suicide and psychoses. At the same time, many struggle to access mental health services and face disruptions in care.
An economic imperative
Insufficient investment in mental health has created major gaps in prevention, care, and support for children, adolescents, and caregivers. Greater and more urgent investment is needed from governments and donor agencies, particularly in low- and middle-income countries where the burden is highest and the resources are most limited.
Mental disorders account for at least 18% of the global disease burden, with projected annual costs of US $6 trillion by 2030. Failing to address the mental health needs of children and adolescents aged 10–17 who have been affected by humanitarian emergencies would result in the equivalent of a global US$203 billion loss of potential lifetime earnings (in US dollars, 2022), driven by reduced school completion, impaired social-emotional skills, and diminished human capital.
These figures highlight that mental health investment is not only compassionate, it is strategic, cost-effective, and essential for achieving sustainable development outcomes.

Our commitment to mental health in emergencies
World Vision’s specific interest in Mental Health and Psychosocial Support (MHPSS) dates back to the 1994 Rwanda Genocide emergency response where staff began to realise that the psychosocial consequences of the war were just as pertinent to peoples’ recovery as was their needs for safety and material aid. However, MHPSS was almost unheard of during that time and it took years for further action to gain momentum.
One of our earliest programs in MHPSS was to develop a tool for measuring depression within the post-conflict Rwanda context. Using this tool, a series of Interpersonal Psychotherapy for Groups (IPTG) programs were developed and later implemented in Uganda, particularly amongst people impacted by HIV/AIDS, with impressive results for sustained symptom reduction.
World Vision’s interest and demand for MHPSS has grown beyond this one approach, now implementing a range of MHPSS programmes in all parts of the world, during emergency responses and in our transformational development programmes. These programmes leverage local resources, faith leaders, and community networks to ensure psychosocial support remains both culturally relevant and sustainable.
Our programmes strengthen community resilience, promote psychological well-being, and ensure access to appropriate care even in the most fragile and crisis-affected settings. By combining evidence-based approaches with community-driven and faith sensitive -informed care, World Vision equips children, families, and caregivers with the skills, hope, and emotional strength needed not only to recover, but to thrive amid adversity.

The Way Forward
As the world marks World Mental Health Day, under the theme “Mental Health in Humanitarian Emergencies,” we are reminded that mental health is not a secondary concern. It is a lifeline in crisis and recovery. Every emergency affects both bodies and minds, and without addressing psychological distress, there can be no true healing, resilience, or sustainable development.
We must renew our collective commitment to invest in mental health for children, caregivers, and communities — ensuring access to prevention, care, and treatment through a continuum of support that leaves no one behind.
Learn more about our work in mental health and psychosocial support.
Phiona Koyiet is the Senior Technical Advisor, Mental Health and Psychosocial World Vision International.