Voices from MEER: Mental health in catastrophes and emergencies cannot be ignored
On World Mental Health Day, MHPSS Advisor Mike Kirakossian calls for integrated, inclusive, and culturally rooted mental health and psychosocial support for children and communities living through emergencies in the Middle East and Eastern Europe region.
9 October 2025
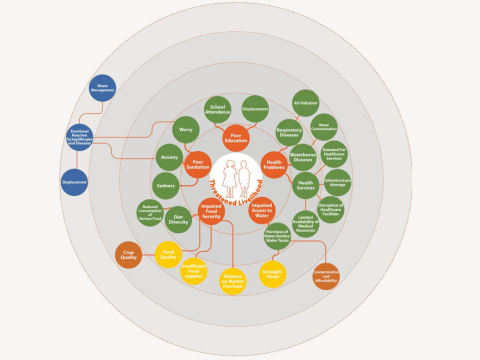
Children and families in the Middle East and Eastern Europe continue to live through conflict, displacement, and sudden disasters. In 2024 alone, we reached 7 million people in response to humanitarian crisis and disasters in the region. In these fragile contexts, we see that mental health support cannot be a secondary concern. It must be seen as a vital part of survival, recovery, and human dignity.
To mark World Mental Health Day, our Mental Health and Psychosocial Support (MHPSS) field office focal points and colleagues from the Regional Impact team reflected on the most urgent mental health and psychosocial needs of children and youth during emergencies. With the theme “Access to services: mental health in catastrophes and emergencies,” what better moment to look at one change that can make the greatest difference?

Removing barriers to mental health care
Across the region, colleagues highlighted a shared truth: stigma remains one of the strongest barriers to care. Many families still view mental health as less important than physical needs, and services are often scarce or of limited quality where they are most needed. In several countries, stigma works hand in hand with the shortage of trained professionals, leaving children and young people without the support they require.
From contexts in Eastern Europe, staff said the lack of tailored and locally available services, together with limited expertise, prevents people from seeking help. Even when programs are in place, they may be difficult to access or unfamiliar in design. Others described how humanitarian settings often fuel a need for quick solutions while true healing requires time, continuity, and compassionate presence. When grief, loss, and instability dominate daily life, short interventions alone cannot rebuild emotional safety.
“Many interventions are still Western in design, focusing on individuals rather than communities. In our contexts, collective and faith-based approaches are often what truly help people recover.” - Staff from Regional Office
Weaving mental health through every aspect of our work
How, then, can we overcome these struggles?
Rather than separating it from other services, mental health should be woven through every aspect of humanitarian and development work.

In the West Bank, conflict and uncertainty has left children exposed to fear and instability that threaten their sense of security. Colleagues emphasised that access to safe spaces, supportive caregivers, and structured opportunities to express emotion are among their most urgent needs. They want to see mental health and psychosocial support, not as a stand-alone service, but fully integrated within schools, community networks, health programs, and protection systems.
Staff from multiple countries noted the importance of training non-specialist workers to provide psychological first aid, integrating mental health into primary health care, and designing flexible, mobile, and culturally grounded models of care. From Romania came a reminder of the healing power of creativity, play, and faith. Creating safe spaces where children can draw, act, and express emotion helps restore their sense of control and belonging after disasters. A holistic and integrated mental health and psychosocial support system that combines counselling, community networks, and trained adults offers the most sustainable way to ensure no child is left without care.
“After disasters, children need psychological first aid, caring adults, and safe spaces to play and express themselves. Art, creativity, and faith help them find hope again.” - Staff from Romania
Together, these voices express a shared conviction. Access to mental health care in emergencies is not about adding new services but about ensuring that support is inclusive, culturally rooted, and present wherever children live, learn, and play. Because even amid catastrophe, every child deserves safety, understanding, and the chance to thrive.
At World Vision MEER, we developed a dedicated MHPSS Road Map for FY 25-30, adapted to the region's unique challenges – including sociocultural complexities, conflict induced adversity, and climate-related shifts – that require tailored interventions and resource allocation to address the diverse mental health needs of children, adolescents, caregivers, and communities.
Mike Kirakossian is the Regional MHPSS Advisor at World Vision’s Middle East and Eastern Europe Office and a licensed clinical psychologist based in Beirut, Lebanon. With over eleven years of humanitarian and development experience, he specialises in psychotraumatology, crisis management, and integrative psychosocial interventions for children, youth, and adults. He also serves as Regional Psychosocial Consultant with the IFRC and teaches in the Child and Adolescent Mental Health Diploma program at the American University of Beirut.